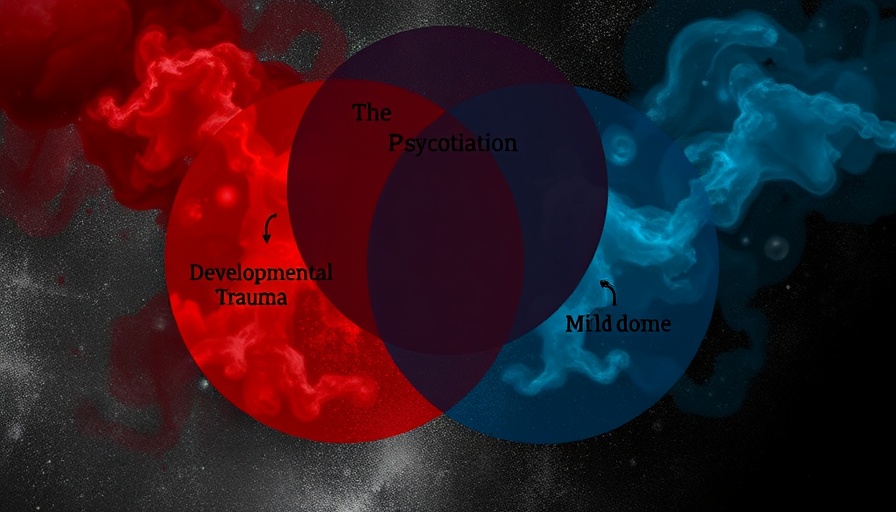
The Intersection of Psychosis, Developmental Trauma, and Dissociation
In the ever-evolving field of mental health, the relationship between psychosis, developmental trauma, and dissociation is an intricate web that is just beginning to be understood. Researchers have sought to clarify how these three elements interact, particularly focusing on individuals who are caught in this often-overlooked intersection.
Historical Overview: The Conceptual Foundations
Historically, figures like Eugen Bleuler introduced important frameworks to understand mental health conditions, notably with his categorization of schizophrenia's four "A's"—ambivalence, autism, affective incongruity, and association disturbances. Although contemporary definitions have moved towards a more rigid categorization of symptoms without explicitly addressing dissociation, the phenomenon remains a crucial aspect of clinical experiences for many. Recent studies indicate that those battling both psychosis and a history of developmental trauma often experience more severe symptoms and worse clinical outcomes. Thus, understanding this overlap is essential for developing effective treatment approaches.
Current Research: Diving into the Evidence Base
Recent studies, including systematic reviews and qualitative research from researchers at University College London, spotlight the importance of this intersection. The systematic review examined literature over a span of decades, analyzing 40 studies and revealing a strong correlation between developmental trauma and psychotic symptoms. Most notably, participants with this dual diagnosis exhibited heightened levels of dissociative experiences. This finding is pivotal, as it raises questions about the psychological mechanisms at play and suggests that it may be crucial to address dissociation in treatments for psychosis.
Understanding Interaction: Trauma and Psychotic Experiences
Developmental trauma—often arising from adverse childhood experiences such as abuse, neglect, or household dysfunction—can create lasting psychological scars. These experiences are not isolated phenomena; they reverberate into adulthood, often manifesting as symptoms of mental health disorders, including various forms of psychosis. This relationship between trauma and psychosis becomes more alarming when dissociation—the psychological process where an individual disconnects from their thoughts, feelings, or sense of identity—enters the narrative. Research indicates that dissociation could act as an intermediary between trauma and psychotic experiences; thus, understanding this connection could lead to more tailored and compassionate treatment strategies.
Qualitative Insights: Voices from the Ground
In tandem with quantitative studies, qualitative research sheds light on the personal experiences of individuals living at this intersection. By conducting semi-structured interviews with participants who have histories of both developmental trauma and subclinical psychosis, researchers captured the nuances of dissociative experiences. The findings reveal how such experiences not only affect mental health but also the social dynamics in which individuals navigate their lives. Engaging with their narratives provides a richer, more humanized understanding of their struggles and resilience.
Future Directions: Towards Holistic Understanding and Treatment
The intricate relationship between psychosis, developmental trauma, and dissociation signals the need for integrated treatment models that address not just the psychotic symptoms but also the underlying trauma and dissociative experiences. Mental health professionals are encouraged to adapt their frameworks to incorporate trauma-informed care that recognizes the impact of early adverse experiences on long-term mental health outcomes. Implementing strategies that include psychotherapy focused on integration and stabilization of dissociative experiences may provide more effective support for those affected.
Common Misconceptions: Breaking Down Barriers to Understanding
One common misconception surrounding psychosis and trauma is the belief that they are wholly separate conditions that do not interact. This misunderstanding can lead to fragmented care and a lack of comprehensive treatment strategies. It is essential to recognize that the interplay of these conditions can exacerbate mental health issues, and treating one without acknowledging or addressing the other may not yield the optimal recovery outcomes.
Call to Action: Embracing Compassionate Mental Health Care
The complexities of mental health require a holistic approach. By acknowledging and addressing the links between psychosis, developmental trauma, and dissociation, mental health professionals can develop more effective and empathetic treatment plans. It is time for those affected to advocate for care that recognizes their unique experiences and challenges. It's not just about managing symptoms—it's about holistic healing and understanding.
 Add Row
Add Row  Add
Add 


Write A Comment